HBO的熱門劇集《最后生還者》(The Last of Us)的觀眾人數以百萬計,人們反復觀看這部劇集,卻很少有人能想到,這部劇集是以現實為基礎。
這部劇的編劇表示,它的前提是一種真菌感染毀滅了整個世界,而事實上,世界衛生組織(World Health Organization)同樣擔心真菌感染問題。
2022年10月,世衛組織發布了第一份真菌“重點病原體”清單,并發出了一系列可怕的警告。世衛組織列出了變得更普遍和更難治療的真菌病原體,目前醫療專業人員只有四類藥物可用于治療這些病原體。
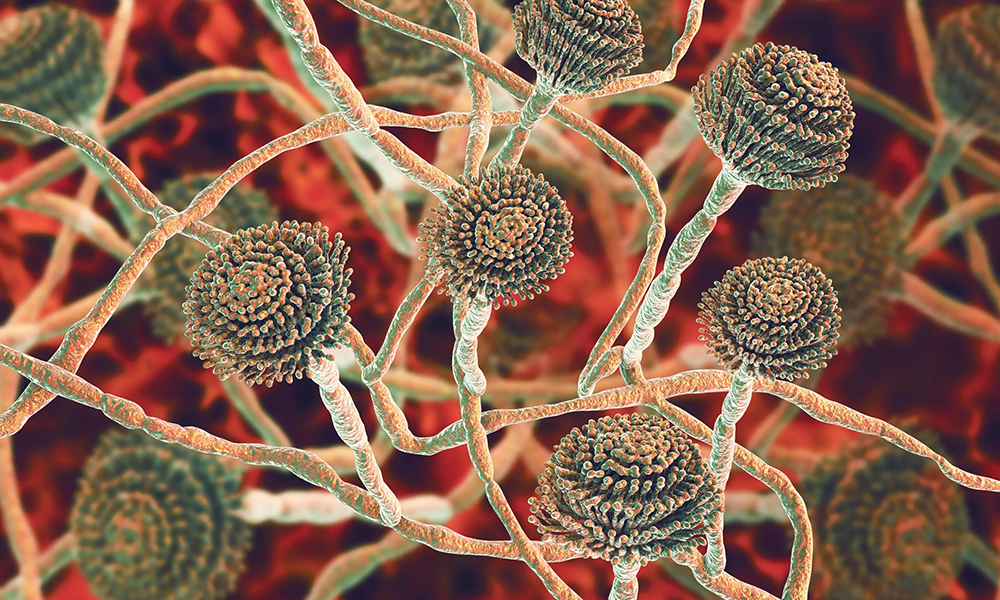
一系列真菌可能引發疾病,這些真菌無處不在,從寬敞的戶外,到室內的表面,甚至人體內,都有真菌存在。真菌感染會引發各種健康問題,包括皮膚感染、哮喘或肺炎等肺部疾病、血流感染、皮癬、腦膜炎或結核菌株等。
雖然許多真菌感染被認為是微不足道的日常小問題,例如腳氣或酵母菌感染等,但其他侵入性感染卻會給免疫力低下的患者或患有嚴重基礎病的患者帶來巨大風險。專家估計,每年約有200萬人死于真菌感染。
“從陰影中出現”
世衛組織抗微生物藥物耐藥性(AMR)事務助理總干事哈南·巴爾基博士在去年10月的新聞稿中表示,當全世界忙于應對新冠的時候,真菌感染“從陰影中出現”,并且耐藥性更強。
因此,世衛組織開始列舉增加對這些病原體的開發研究以確定它們的危險性和抗藥性的理由。
世衛組織在公布真菌“重點病原體”清單時強調,目前對于這些病原體沒有足夠的證據或知識,能夠充分了解這些病原體對公共健康帶來的“負擔”。
然而,聯合國官員表示,各國可以開始采取措施,例如增強實驗室能力,保證現有治療藥物的公平分配等,應對可能危險的真菌感染。
我們以前為何從未聽說過真菌感染的危險?
專家對《財富》雜志表示,真菌感染長期以來就在我們的眼皮底下,卻沒有引起公共健康部門的關注。
傳染病學專家、倫敦大學學院附屬醫院(University College London Hospitals)的真菌感染負責人尼爾·斯通博士在電話中表示:“一想到真菌感染,我們就會想起一些奇怪或令人尷尬的事情,這些都是繁瑣和膚淺的問題。一直以來,我們都忽視了這些疾病,人們可能要花數十年時間才能重視起來。”
曼徹斯特大學(University of Manchester)傳染病學教授大衛·丹寧補充道,真菌感染不僅被一個單調的名稱所掩蓋,甚至不屬于任何特定公共部門的職權范圍。
他表示,這是因為真菌感染疾病跨越了眾多醫療領域,而且經常會被誤診。他指出,感染和死于真菌感染的人數在不斷增多。病例數增加有許多原因,包括:壽命延長、氣候變化、旅行和抗藥性等。
倫敦大學學院的斯通表示,抗藥性是關鍵,因為醫療專業人員用于治療真菌病的有限藥物,經常在人類和動物體內被過度使用。
真菌感染多久會成為一個嚴重問題?
然而,有一些好消息。斯通表示,真菌感染人數不會像新冠疫情一樣“爆炸性”增長。
他還表示,新冠疫情已經證明,在必要的時候,醫學界能迅速團結起來解決問題,但他指出,開發更好的診斷方法和擴充“少得可憐的”藥物清單,必須是首要任務。
曼徹斯特大學的丹寧解釋稱,應對真菌感染人數增加的措施,將以不同的速度展開。丹寧同時擔任全球真菌感染行動組織(Global Action for Fungal Infections,GAFFI)的首席執行官。
他對《財富》雜志表示:“在有些方面,我們可以迅速行動,以產生巨大的影響。快速診斷就是其中之一。我們可以指導人們如何簡單地使用檢測試劑,其單價只有約4美元。”
他表示,從長遠來看,為了減少誤診和確定最容易真菌感染的患者群體,培訓真菌感染領域的醫生和臨床與實驗室參與是關鍵。之后,公共健康部門就可以更輕松地收集和分享相關數據。
公眾需要做些什么?
專家表示,首先人們要認識到,真菌感染不只是腳氣。
除此之外,丹寧教授認為,有一些群體可能需要向醫療專業人員討論自己的癥狀。
他說道:“如果你免疫力低下,或許你有胸部或皮膚問題,如果你是一名女性,經常感染酵母菌,下一次看醫生的時候不要只是購買類固醇藥膏或處方藥,而是問問醫生:‘這是真菌感染嗎?’真菌感染檢查沒有什么特別,只是這并不是常規檢查。公眾需要提高對于真菌感染疾病的認識。”(財富中文網)
翻譯:劉進龍
審校:汪皓
HBO的熱門劇集《最后生還者》(The Last of Us)的觀眾人數以百萬計,人們反復觀看這部劇集,卻很少有人能想到,這部劇集是以現實為基礎。
這部劇的編劇表示,它的前提是一種真菌感染毀滅了整個世界,而事實上,世界衛生組織(World Health Organization)同樣擔心真菌感染問題。
2022年10月,世衛組織發布了第一份真菌“重點病原體”清單,并發出了一系列可怕的警告。世衛組織列出了變得更普遍和更難治療的真菌病原體,目前醫療專業人員只有四類藥物可用于治療這些病原體。
一系列真菌可能引發疾病,這些真菌無處不在,從寬敞的戶外,到室內的表面,甚至人體內,都有真菌存在。真菌感染會引發各種健康問題,包括皮膚感染、哮喘或肺炎等肺部疾病、血流感染、皮癬、腦膜炎或結核菌株等。
雖然許多真菌感染被認為是微不足道的日常小問題,例如腳氣或酵母菌感染等,但其他侵入性感染卻會給免疫力低下的患者或患有嚴重基礎病的患者帶來巨大風險。專家估計,每年約有200萬人死于真菌感染。
“從陰影中出現”
世衛組織抗微生物藥物耐藥性(AMR)事務助理總干事哈南·巴爾基博士在去年10月的新聞稿中表示,當全世界忙于應對新冠的時候,真菌感染“從陰影中出現”,并且耐藥性更強。
因此,世衛組織開始列舉增加對這些病原體的開發研究以確定它們的危險性和抗藥性的理由。
世衛組織在公布真菌“重點病原體”清單時強調,目前對于這些病原體沒有足夠的證據或知識,能夠充分了解這些病原體對公共健康帶來的“負擔”。
然而,聯合國官員表示,各國可以開始采取措施,例如增強實驗室能力,保證現有治療藥物的公平分配等,應對可能危險的真菌感染。
我們以前為何從未聽說過真菌感染的危險?
專家對《財富》雜志表示,真菌感染長期以來就在我們的眼皮底下,卻沒有引起公共健康部門的關注。
傳染病學專家、倫敦大學學院附屬醫院(University College London Hospitals)的真菌感染負責人尼爾·斯通博士在電話中表示:“一想到真菌感染,我們就會想起一些奇怪或令人尷尬的事情,這些都是繁瑣和膚淺的問題。一直以來,我們都忽視了這些疾病,人們可能要花數十年時間才能重視起來。”
曼徹斯特大學(University of Manchester)傳染病學教授大衛·丹寧補充道,真菌感染不僅被一個單調的名稱所掩蓋,甚至不屬于任何特定公共部門的職權范圍。
他表示,這是因為真菌感染疾病跨越了眾多醫療領域,而且經常會被誤診。他指出,感染和死于真菌感染的人數在不斷增多。病例數增加有許多原因,包括:壽命延長、氣候變化、旅行和抗藥性等。
倫敦大學學院的斯通表示,抗藥性是關鍵,因為醫療專業人員用于治療真菌病的有限藥物,經常在人類和動物體內被過度使用。
真菌感染多久會成為一個嚴重問題?
然而,有一些好消息。斯通表示,真菌感染人數不會像新冠疫情一樣“爆炸性”增長。
他還表示,新冠疫情已經證明,在必要的時候,醫學界能迅速團結起來解決問題,但他指出,開發更好的診斷方法和擴充“少得可憐的”藥物清單,必須是首要任務。
曼徹斯特大學的丹寧解釋稱,應對真菌感染人數增加的措施,將以不同的速度展開。丹寧同時擔任全球真菌感染行動組織(Global Action for Fungal Infections,GAFFI)的首席執行官。
他對《財富》雜志表示:“在有些方面,我們可以迅速行動,以產生巨大的影響。快速診斷就是其中之一。我們可以指導人們如何簡單地使用檢測試劑,其單價只有約4美元。”
他表示,從長遠來看,為了減少誤診和確定最容易真菌感染的患者群體,培訓真菌感染領域的醫生和臨床與實驗室參與是關鍵。之后,公共健康部門就可以更輕松地收集和分享相關數據。
公眾需要做些什么?
專家表示,首先人們要認識到,真菌感染不只是腳氣。
除此之外,丹寧教授認為,有一些群體可能需要向醫療專業人員討論自己的癥狀。
他說道:“如果你免疫力低下,或許你有胸部或皮膚問題,如果你是一名女性,經常感染酵母菌,下一次看醫生的時候不要只是購買類固醇藥膏或處方藥,而是問問醫生:‘這是真菌感染嗎?’真菌感染檢查沒有什么特別,只是這并不是常規檢查。公眾需要提高對于真菌感染疾病的認識。”(財富中文網)
翻譯:劉進龍
審校:汪皓
The millions of viewers who kicked back and watched HBO’s hit series The Last of Us are unlikely to think the show is grounded in much reality.
However, the drama’s writer has defended the premise?that the world could be brought to its knees by a mere fungal infection—and as it turns out, the World Health Organization is worried about it too.
In October 2022, the WHO released the first-ever list of fungal “priority pathogens,” as well as a series of stark warnings. The body outlined that fungal pathogens are becoming both more common and more resistant to treatment, with health professionals having just four classes of medicine available to combat them.
Diseases can be brought on by a range of fungi found everywhere?from the great outdoors to indoor surfaces to inside the human body. These can develop into a raft of health problems including skin infections, lung conditions such as asthma or pneumonia, bloodstream infections, ringworm, meningitis, or strains of tuberculosis.
And although many fungal infections are seen as minor everyday problems—such as athlete’s foot or yeast infections—other invasive forms pose a major risk to immunocompromised patients or those with severe underlying health conditions. Experts estimate that around 2 million people die of fungal infections every year.
‘Emerging from the shadows’
While the world was busy battling COVID, fungal infections began “emerging from the shadows” in more treatment-resistant forms, Dr. Hanan Balkhy, the WHO’s assistant director-general of antimicrobial resistance (AMR), said in an October news release.
As a result, the the organization has begun outlining the case for increasing research and development into these pathogens to establish how dangerous and drug-proof they are.
The WHO emphasized when it published its list of priority fungi that there currently isn’t enough evidence or knowledge of these pathogens to fully understand the “burden” they could have on public health.
However, officials at the U.N. agency said countries could get a head start against potentially dangerous fungal infections by taking steps like strengthening their laboratory capacities and ensuring equitable access to existing treatments.
Why haven’t we heard about this before?
Fungal infections have long been hiding in plain sight and slipping through the cracks of public health bodies, experts told Fortune.
“When we think of fungal infections we think of something a bit weird or embarrassing, something that’s trivial and superficial,” Dr. Neil Stone, a specialist in infectious diseases and University College London Hospitals’ fungal infections lead, said in a phone call. “There’s been a legacy of neglect in looking at these diseases, and it’s taken decades to get people to pay attention.”
As well as masquerading behind a humdrum title, these infections haven’t fallen under the remit of any specific public body to address, added David Denning, a professor of infectious diseases at the University of Manchester.
That’s because these diseases span a vast range of practices and are also often misdiagnosed, he said, noting that the number of people contracting and dying of fungal infections is only increasing. The case numbers are going up because of a range of factors: longer life spans, climate change, travel, and resistance to drugs.
Drug resistance is a key issue, added UCL’s Stone, because the limited arsenal medical professionals do have to fight fungal disease is often overused in both humans and animals.
How quickly will this be a problem?
However, there is some good news. Stone said it’s unlikely the rise in these infections will be anywhere near as “explosive” as the COVID pandemic.
He added that the coronavirus outbreak proved how quickly the medical community can come together to troubleshoot when needed, but noted that developing better diagnosis streams and expanding a “pitiful” repertoire of drugs must be top priorities.
Moves to combat the rise of fungal infections will proceed at varying paces, explained Manchester University’s Denning, who also serves as chief executive of Global Action for Fungal Infections (GAFFI).
“There are things we can do quickly which have a big impact,” he told Fortune. “Rapid diagnostics is one of them—we can teach someone how to use a test really easily, and they only cost about $4 each.”
In the long term, training doctors in the field and linking clinical and laboratory engagement is essential, in order to cut down on misdiagnosis and establish which groups of patients are most susceptible to which disease, he added. From there data can be more easily collected and shared by public health bodies.
What does the public need to do?
Being aware that fungal diseases are more than just athlete’s foot is a good place to start, the experts said.
On top of this, there are a few groups of people who might need to chat to a health professional about their symptoms, added Professor Denning.
“If you’re immunocompromised, maybe you have a bad chest or bad skin, or you’re a woman who suffers with recurring yeast infections, then next time you go to the doctor instead of getting a steroid cream or prescription, ask: ‘Is this a fungal infection?'” he said. “The tests are very similar, they’re just not done as routinely. There just needs to be a general awareness of these diseases.”






