2022年,在美國(guó)得克薩斯州的圣安東尼奧,阿圖羅·博尼拉博士小心翼翼地將一只外耳植入到一名20歲女子的身上,這名女子天生缺少一只外耳。右側(cè)植入的外耳是按照她左側(cè)外耳的大小和形狀構(gòu)建的。
博尼拉是一位有著25年以上經(jīng)驗(yàn)的小耳畸形外科醫(yī)生(治療耳部先天缺陷的醫(yī)生),也是該領(lǐng)域公認(rèn)的專家,對(duì)他來(lái)說(shuō),這樣的手術(shù)很常規(guī)。但這個(gè)案例令人意想不到的點(diǎn)在于這是他首次將3D打印的耳朵(利用該女子自身的軟骨細(xì)胞)植入人體。
博尼拉告訴我,植入手術(shù)“非常順利”。總而言之,說(shuō)手術(shù)非常順利,那絕對(duì)是輕描淡寫。
從近乎虛構(gòu)走向萌芽,再走到真實(shí)的科學(xué)研究,3D生物打印應(yīng)用于醫(yī)學(xué)研究的方方面面都取得了進(jìn)展,如今,3D生物打印正在實(shí)踐方面取得進(jìn)步。雖然進(jìn)展緩慢,一些宏大的3D計(jì)劃設(shè)定的目標(biāo)日期是在幾十年后,但3D生物打印著實(shí)取得了實(shí)實(shí)在在的進(jìn)步。
位于以色列的特拉維夫大學(xué)(Tel Aviv University)的組織工程和再生醫(yī)學(xué)主任塔爾·德維爾教授說(shuō):“我認(rèn)為在10年內(nèi),我們能夠打印出用于移植的器官。我們將從像皮膚和軟骨這樣的簡(jiǎn)單器官開(kāi)始,然后轉(zhuǎn)向更復(fù)雜的組織——最終的目標(biāo)是打印心臟、肝臟和腎臟。”
3D生物打印的未來(lái)
這聽(tīng)起來(lái)很玄乎,但已經(jīng)成為現(xiàn)實(shí)了。多層皮膚、骨骼、肌肉結(jié)構(gòu)、血管、視網(wǎng)膜組織,甚至微器官都已經(jīng)被3D打印出來(lái)了。雖然這些打印出來(lái)的組織還沒(méi)有被批準(zhǔn)用于人體,但科學(xué)發(fā)展的進(jìn)程令人嘆為觀止——博尼拉的耳朵手術(shù)是首次將3D打印的耳朵(利用活細(xì)胞)植入人體,這是一大里程碑事件。
根據(jù)2022年的一份摘要和仿生胰腺的制造者米哈爾·弗紹瓦博士的介紹,波蘭的研究人員生物打印了一個(gè)具備各種功能的胰腺原型,在觀察的兩周時(shí)間里,豬體內(nèi)血液流動(dòng)穩(wěn)定。United Therapeutics Corporation已經(jīng) 3D打印了一個(gè)人類肺部支架,毛細(xì)血管全長(zhǎng)達(dá)4,000千米,還有2億個(gè)肺泡(微小的氣囊),可以在動(dòng)物模型中進(jìn)行氧氣交換,這是制造可耐受、可移植的人類肺部的關(guān)鍵一步,該公司的目標(biāo)是讓打印的人類肺部支架在五年內(nèi)被批準(zhǔn)用于人體試驗(yàn)。
在維克森林大學(xué)再生醫(yī)學(xué)研究所(Wake Forest University Institute for Regenerative Medicine),科學(xué)家們開(kāi)發(fā)了一種移動(dòng)式皮膚生物打印系統(tǒng)。在不久的將來(lái),他們預(yù)計(jì)能夠直接把打印機(jī)推到傷口難以愈合(例如燒傷)的患者床邊,然后掃描和測(cè)量傷口面積,并將3D打印的皮膚一層一層地直接打印到患者的傷口表面。他們還進(jìn)行了深入研究,3D打印的骨骼肌構(gòu)建體已被證明可以在嚙齒動(dòng)物身上實(shí)現(xiàn)收縮功能,而且脛骨前肌80%以上先前喪失的肌肉功能能夠在八周內(nèi)得到恢復(fù)。
德維爾自己的實(shí)驗(yàn)室已經(jīng)3D打印出一顆“兔子心臟大小”的心臟,正如他所說(shuō)的,這顆心臟充滿細(xì)胞、心室和主要血管,還可以和心臟一樣跳動(dòng)。教授指出,盡管按照比例放大的過(guò)程非常復(fù)雜,但打印全尺寸的人類心臟需要采用同樣的基本技術(shù)。“我們?nèi)缃裾谘芯科鸩?xì)胞、心房肌細(xì)胞和心室肌細(xì)胞。”德維爾表示。“目前看起來(lái)進(jìn)展不錯(cuò)。我相信這就是3D生物打印的未來(lái)。”
3D生物打印是如何工作的

3D打印人體器官這樣的概念令人震驚。根據(jù)美國(guó)聯(lián)邦衛(wèi)生資源和服務(wù)管理局(Health Resources and Services Administration)的數(shù)據(jù),目前有近10.6萬(wàn)美國(guó)人正在等待器官移植,每天有17人在等待器官移植時(shí)死亡。利用患者自身細(xì)胞培育器官的3D打印技術(shù)不僅可能導(dǎo)致等待器官移植的患者減少,還會(huì)大大降低器官移植排異的幾率,并可能消除終生服用對(duì)身體有害的免疫抑制藥物的需求。
斯坦福大學(xué)(Stanford University)的生物工程系助理教授馬克·斯凱拉-斯科特說(shuō):“兩項(xiàng)(3D)技術(shù)為組織工程領(lǐng)域帶來(lái)重大革新,一是將不同類型的細(xì)胞放置在精確的位置以構(gòu)建復(fù)雜組織,二是整合血管以輸送必要的氧氣和營(yíng)養(yǎng)物質(zhì)來(lái)保持細(xì)胞存活。在過(guò)去的20年里,該領(lǐng)域發(fā)展非常迅速,從打印膀胱到如今能夠打印帶有可以與泵相連的血管的復(fù)雜組織,以及類似于帶有集成各種心肌細(xì)胞的心臟組織的復(fù)雜3D模型。”
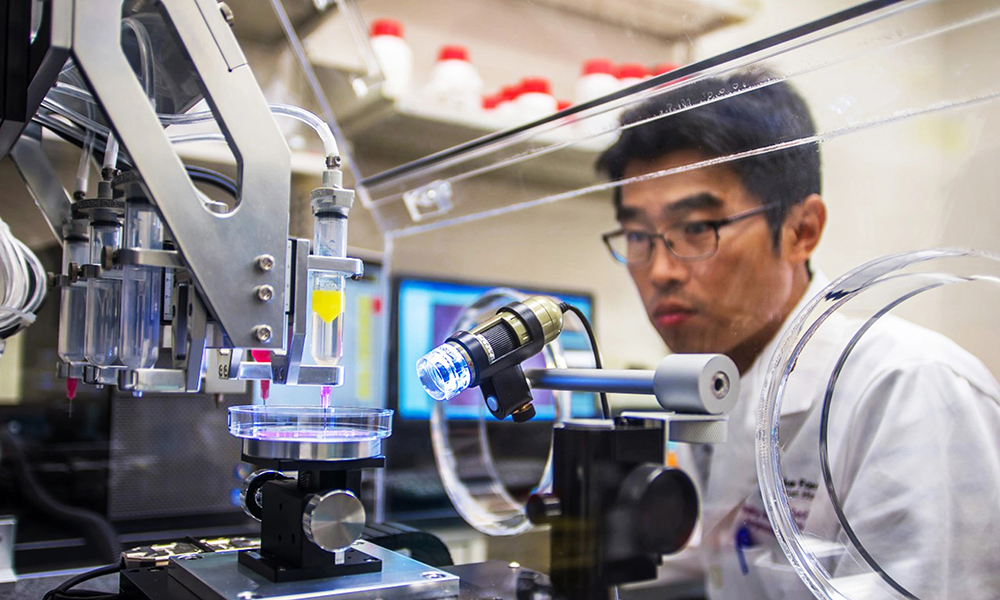
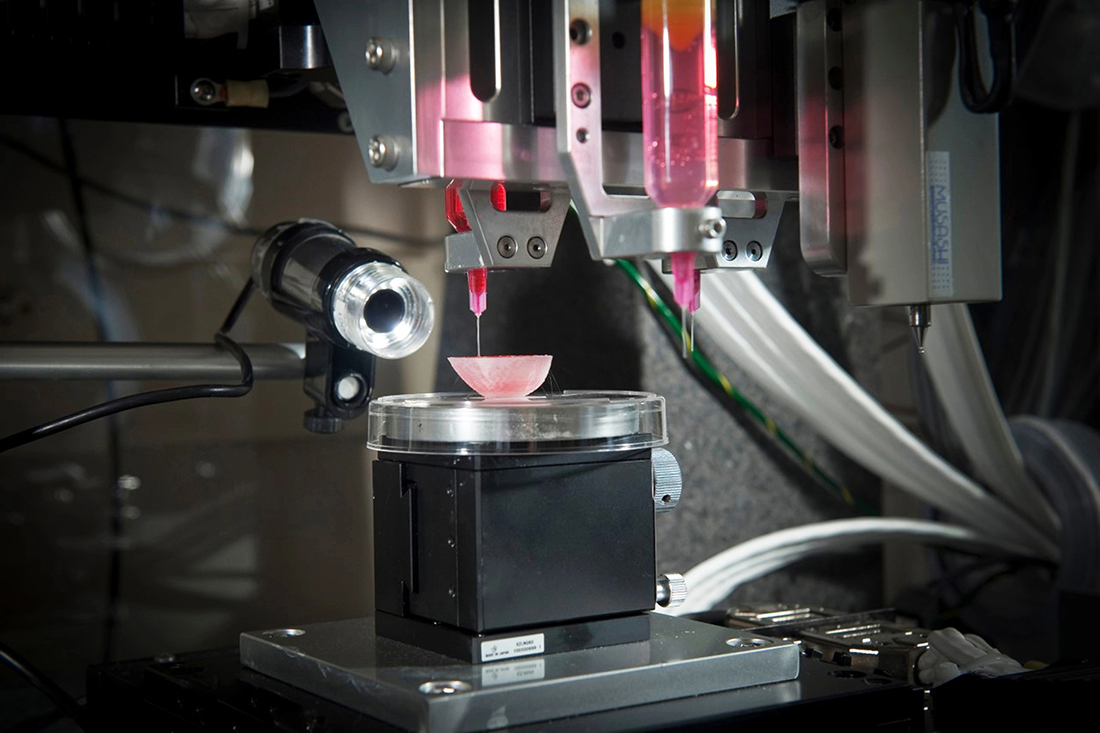
在3D生物打印中,最重要的部分就是細(xì)胞。就3D生物打印過(guò)程而言,首先是生成研究人員想要生物打印的細(xì)胞,然后指示它們形成特定器官細(xì)胞類型。然后,這些細(xì)胞被制成能夠打印的活墨水或生物墨水,包括將它們與明膠或海藻酸鹽等材料混合,以使它們具有類似牙膏的粘度。斯坦福大學(xué)的實(shí)驗(yàn)室正在研究,高密度地?cái)D在一起的干細(xì)胞是如何自然地形成這種粘度的,這可能會(huì)導(dǎo)致3D打印器官完全由患者自身的細(xì)胞制成。
斯凱拉-斯科特指出,生物墨水被裝入注射器,然后“就像蛋糕上的糖霜”一樣從噴頭中擠出。這是真正的3D生物打印過(guò)程,它通常包括放置不同類型的細(xì)胞,每個(gè)細(xì)胞都被裝入不同的噴頭。(德維爾說(shuō),打印這個(gè)迷你心臟花了大約4個(gè)小時(shí)。)一旦完成,組織有時(shí)會(huì)被連接到一個(gè)泵上,這樣就可以為該組織輸送氧氣和營(yíng)養(yǎng)物質(zhì)。隨著時(shí)間的推移,該組織就會(huì)自行發(fā)育,成熟度會(huì)不斷提高,功能也會(huì)更加完善。
這個(gè)大致的過(guò)程,雖然在這里被大大簡(jiǎn)化了,但阿圖羅·博尼拉醫(yī)生在得克薩斯州將這個(gè)過(guò)程的產(chǎn)物——打印的外耳——植入患者。在以前的大多數(shù)小耳畸形手術(shù)里,博尼拉會(huì)從患者肋骨上提取軟骨,將其雕刻成耳朵的大致形狀。這一次,博尼拉在患者的另一只耳朵上進(jìn)行了一個(gè)小的活檢,從活檢中提取的軟骨細(xì)胞被培養(yǎng)成數(shù)十億個(gè)細(xì)胞,這些細(xì)胞被3D打印成了新的植入物。
博尼拉說(shuō):“與任何研究一樣,為了嘗試改進(jìn)這項(xiàng)技術(shù),未來(lái)的患者可能會(huì)經(jīng)歷迭代。我們不確定這將在何時(shí)成為主要治療方法,但該技術(shù)的未來(lái)是非常激動(dòng)人心的。”
3D打印的優(yōu)勢(shì)
維克森林大學(xué)的科學(xué)家多年來(lái)一直在實(shí)驗(yàn)室培育器官和組織。他們?cè)趯?shí)驗(yàn)室里用3D打印技術(shù)制造了一個(gè)迷你腎臟和一個(gè)迷你肝臟。下一個(gè)挑戰(zhàn):更大的、可以更充分地模擬器官功能的實(shí)心結(jié)構(gòu)。“在器官尺寸上,我們離實(shí)現(xiàn)這一目標(biāo)還有很長(zhǎng)一段路要走。”哈佛大學(xué)(Harvard University)懷斯生物啟發(fā)工程研究所(Biologically Inspired Engineering)的教授詹妮弗·劉易斯表示。
“我們已經(jīng)能夠打印出像皮膚這樣的平面結(jié)構(gòu),像血管這樣的管狀結(jié)構(gòu),或者像膀胱這樣的空心非管狀器官。”維克森林研究所的創(chuàng)始主任安東尼·阿塔拉說(shuō)。“由于血管和營(yíng)養(yǎng)方面的挑戰(zhàn)”,打印更大的實(shí)心器官是不同的,畢竟“每厘米就有非常多細(xì)胞。”
在細(xì)胞制造的某些方面,還存在質(zhì)量問(wèn)題。科學(xué)家們已經(jīng)可以從干細(xì)胞中制造出心肌細(xì)胞,但制造出的心肌細(xì)胞無(wú)法像你的心肌細(xì)胞那樣強(qiáng)烈地跳動(dòng)。肝細(xì)胞(代謝)和腎細(xì)胞(濾液攝取)的情況也是如此。斯凱拉-斯科特稱:“從某些方面講,3D生物打印領(lǐng)域正在等待基礎(chǔ)生物學(xué)家取得重大突破。”
還有一個(gè)問(wèn)題是數(shù)量問(wèn)題。制造一顆心臟需要“數(shù)十億個(gè)細(xì)胞——而且需要不同的細(xì)胞,甚至是不同的心肌細(xì)胞。”塔爾·德維爾說(shuō)道。根據(jù)斯凱拉-斯科特的說(shuō)法,要為一個(gè)器官制造足夠的細(xì)胞,制造廠需要一個(gè)10升的攪拌缸,每天可能要花費(fèi)5,000美元,而且需要連續(xù)幾個(gè)月才能夠完成。最終目標(biāo)是每個(gè)月培育上千個(gè)器官,而不是一個(gè)器官。
3D Bio Therapeutics的首席執(zhí)行官及聯(lián)合創(chuàng)始人丹·科恩表示,除此之外,還有組織如何融入人體以及如何得到人體的支持等問(wèn)題,包括復(fù)雜的血管、神經(jīng)和多種細(xì)胞類型網(wǎng)絡(luò)。“這并不是說(shuō)這一點(diǎn)無(wú)法做到。”科恩說(shuō),他20年前就開(kāi)始在生物打印領(lǐng)域工作,當(dāng)時(shí)這個(gè)領(lǐng)域連個(gè)正式的名字都沒(méi)有。“我對(duì)生物打印和再生醫(yī)學(xué)的廣泛應(yīng)用抱有很大希望。”
就短期而言,進(jìn)展也是非常顯著的。劉易斯表示,哈佛大學(xué)的研究人員從人類多能干細(xì)胞中培育出心肌細(xì)胞,然后將它們植入帶有傳感器(這些傳感器可以追蹤跳動(dòng)的組織)的生物工程芯片上。這種3D打印的芯片上的心臟能夠用于測(cè)試各種心臟藥物的潛在毒副作用,并可能減輕對(duì)動(dòng)物試驗(yàn)的需求。(類似的芯片上的肌萎縮性側(cè)索硬化癥技術(shù)正在被用于篩選候選藥物,這樣也可以更好地了解這種疾病的潛在機(jī)制。)
維克森林大學(xué)的阿塔拉說(shuō):“3D打印機(jī)有幾大優(yōu)點(diǎn)。首先是能夠擴(kuò)大規(guī)模,因?yàn)槟憧梢杂么蛴C(jī)自動(dòng)化打印(組織和器官),而不是手工一次完成一個(gè)。其次是能夠確保精確度。我們可以更精確地將細(xì)胞放置在需要它們的地方。”
再有一點(diǎn)就是能夠降低整體成本,這是因?yàn)?D打印允許加大規(guī)模。這就是阿塔拉所說(shuō)的“可重復(fù)性”(一種可以反復(fù)制造相同結(jié)構(gòu)的方法)。在器官移植方面,由患者自身細(xì)胞制成的新器官能夠大大降低排異反應(yīng)的可能性。
大多數(shù)研究人員認(rèn)為,全尺寸3D打印人體器官移植還需要20年到30年的時(shí)間。“展望未來(lái),我們將無(wú)需接受心臟捐贈(zèng),也無(wú)需接受肝臟捐贈(zèng)。”德維爾說(shuō)。“這是我的觀點(diǎn),而且我很樂(lè)觀,我認(rèn)為在不到20年的時(shí)間里,就會(huì)出現(xiàn)打印的器官被植入患者體內(nèi)。”這是科學(xué)在發(fā)揮作用,而不是科幻小說(shuō)。(財(cái)富中文網(wǎng))
譯者:中慧言-王芳
2022年,在美國(guó)得克薩斯州的圣安東尼奧,阿圖羅·博尼拉博士小心翼翼地將一只外耳植入到一名20歲女子的身上,這名女子天生缺少一只外耳。右側(cè)植入的外耳是按照她左側(cè)外耳的大小和形狀構(gòu)建的。
博尼拉是一位有著25年以上經(jīng)驗(yàn)的小耳畸形外科醫(yī)生(治療耳部先天缺陷的醫(yī)生),也是該領(lǐng)域公認(rèn)的專家,對(duì)他來(lái)說(shuō),這樣的手術(shù)很常規(guī)。但這個(gè)案例令人意想不到的點(diǎn)在于這是他首次將3D打印的耳朵(利用該女子自身的軟骨細(xì)胞)植入人體。
博尼拉告訴我,植入手術(shù)“非常順利”。總而言之,說(shuō)手術(shù)非常順利,那絕對(duì)是輕描淡寫。
從近乎虛構(gòu)走向萌芽,再走到真實(shí)的科學(xué)研究,3D生物打印應(yīng)用于醫(yī)學(xué)研究的方方面面都取得了進(jìn)展,如今,3D生物打印正在實(shí)踐方面取得進(jìn)步。雖然進(jìn)展緩慢,一些宏大的3D計(jì)劃設(shè)定的目標(biāo)日期是在幾十年后,但3D生物打印著實(shí)取得了實(shí)實(shí)在在的進(jìn)步。
位于以色列的特拉維夫大學(xué)(Tel Aviv University)的組織工程和再生醫(yī)學(xué)主任塔爾·德維爾教授說(shuō):“我認(rèn)為在10年內(nèi),我們能夠打印出用于移植的器官。我們將從像皮膚和軟骨這樣的簡(jiǎn)單器官開(kāi)始,然后轉(zhuǎn)向更復(fù)雜的組織——最終的目標(biāo)是打印心臟、肝臟和腎臟。”
3D生物打印的未來(lái)
這聽(tīng)起來(lái)很玄乎,但已經(jīng)成為現(xiàn)實(shí)了。多層皮膚、骨骼、肌肉結(jié)構(gòu)、血管、視網(wǎng)膜組織,甚至微器官都已經(jīng)被3D打印出來(lái)了。雖然這些打印出來(lái)的組織還沒(méi)有被批準(zhǔn)用于人體,但科學(xué)發(fā)展的進(jìn)程令人嘆為觀止——博尼拉的耳朵手術(shù)是首次將3D打印的耳朵(利用活細(xì)胞)植入人體,這是一大里程碑事件。
根據(jù)2022年的一份摘要和仿生胰腺的制造者米哈爾·弗紹瓦博士的介紹,波蘭的研究人員生物打印了一個(gè)具備各種功能的胰腺原型,在觀察的兩周時(shí)間里,豬體內(nèi)血液流動(dòng)穩(wěn)定。United Therapeutics Corporation已經(jīng) 3D打印了一個(gè)人類肺部支架,毛細(xì)血管全長(zhǎng)達(dá)4,000千米,還有2億個(gè)肺泡(微小的氣囊),可以在動(dòng)物模型中進(jìn)行氧氣交換,這是制造可耐受、可移植的人類肺部的關(guān)鍵一步,該公司的目標(biāo)是讓打印的人類肺部支架在五年內(nèi)被批準(zhǔn)用于人體試驗(yàn)。
在維克森林大學(xué)再生醫(yī)學(xué)研究所(Wake Forest University Institute for Regenerative Medicine),科學(xué)家們開(kāi)發(fā)了一種移動(dòng)式皮膚生物打印系統(tǒng)。在不久的將來(lái),他們預(yù)計(jì)能夠直接把打印機(jī)推到傷口難以愈合(例如燒傷)的患者床邊,然后掃描和測(cè)量傷口面積,并將3D打印的皮膚一層一層地直接打印到患者的傷口表面。他們還進(jìn)行了深入研究,3D打印的骨骼肌構(gòu)建體已被證明可以在嚙齒動(dòng)物身上實(shí)現(xiàn)收縮功能,而且脛骨前肌80%以上先前喪失的肌肉功能能夠在八周內(nèi)得到恢復(fù)。
德維爾自己的實(shí)驗(yàn)室已經(jīng)3D打印出一顆“兔子心臟大小”的心臟,正如他所說(shuō)的,這顆心臟充滿細(xì)胞、心室和主要血管,還可以和心臟一樣跳動(dòng)。教授指出,盡管按照比例放大的過(guò)程非常復(fù)雜,但打印全尺寸的人類心臟需要采用同樣的基本技術(shù)。“我們?nèi)缃裾谘芯科鸩?xì)胞、心房肌細(xì)胞和心室肌細(xì)胞。”德維爾表示。“目前看起來(lái)進(jìn)展不錯(cuò)。我相信這就是3D生物打印的未來(lái)。”
3D生物打印是如何工作的
3D打印人體器官這樣的概念令人震驚。根據(jù)美國(guó)聯(lián)邦衛(wèi)生資源和服務(wù)管理局(Health Resources and Services Administration)的數(shù)據(jù),目前有近10.6萬(wàn)美國(guó)人正在等待器官移植,每天有17人在等待器官移植時(shí)死亡。利用患者自身細(xì)胞培育器官的3D打印技術(shù)不僅可能導(dǎo)致等待器官移植的患者減少,還會(huì)大大降低器官移植排異的幾率,并可能消除終生服用對(duì)身體有害的免疫抑制藥物的需求。
斯坦福大學(xué)(Stanford University)的生物工程系助理教授馬克·斯凱拉-斯科特說(shuō):“兩項(xiàng)(3D)技術(shù)為組織工程領(lǐng)域帶來(lái)重大革新,一是將不同類型的細(xì)胞放置在精確的位置以構(gòu)建復(fù)雜組織,二是整合血管以輸送必要的氧氣和營(yíng)養(yǎng)物質(zhì)來(lái)保持細(xì)胞存活。在過(guò)去的20年里,該領(lǐng)域發(fā)展非常迅速,從打印膀胱到如今能夠打印帶有可以與泵相連的血管的復(fù)雜組織,以及類似于帶有集成各種心肌細(xì)胞的心臟組織的復(fù)雜3D模型。”
在3D生物打印中,最重要的部分就是細(xì)胞。就3D生物打印過(guò)程而言,首先是生成研究人員想要生物打印的細(xì)胞,然后指示它們形成特定器官細(xì)胞類型。然后,這些細(xì)胞被制成能夠打印的活墨水或生物墨水,包括將它們與明膠或海藻酸鹽等材料混合,以使它們具有類似牙膏的粘度。斯坦福大學(xué)的實(shí)驗(yàn)室正在研究,高密度地?cái)D在一起的干細(xì)胞是如何自然地形成這種粘度的,這可能會(huì)導(dǎo)致3D打印器官完全由患者自身的細(xì)胞制成。
斯凱拉-斯科特指出,生物墨水被裝入注射器,然后“就像蛋糕上的糖霜”一樣從噴頭中擠出。這是真正的3D生物打印過(guò)程,它通常包括放置不同類型的細(xì)胞,每個(gè)細(xì)胞都被裝入不同的噴頭。(德維爾說(shuō),打印這個(gè)迷你心臟花了大約4個(gè)小時(shí)。)一旦完成,組織有時(shí)會(huì)被連接到一個(gè)泵上,這樣就可以為該組織輸送氧氣和營(yíng)養(yǎng)物質(zhì)。隨著時(shí)間的推移,該組織就會(huì)自行發(fā)育,成熟度會(huì)不斷提高,功能也會(huì)更加完善。
這個(gè)大致的過(guò)程,雖然在這里被大大簡(jiǎn)化了,但阿圖羅·博尼拉醫(yī)生在得克薩斯州將這個(gè)過(guò)程的產(chǎn)物——打印的外耳——植入患者。在以前的大多數(shù)小耳畸形手術(shù)里,博尼拉會(huì)從患者肋骨上提取軟骨,將其雕刻成耳朵的大致形狀。這一次,博尼拉在患者的另一只耳朵上進(jìn)行了一個(gè)小的活檢,從活檢中提取的軟骨細(xì)胞被培養(yǎng)成數(shù)十億個(gè)細(xì)胞,這些細(xì)胞被3D打印成了新的植入物。
博尼拉說(shuō):“與任何研究一樣,為了嘗試改進(jìn)這項(xiàng)技術(shù),未來(lái)的患者可能會(huì)經(jīng)歷迭代。我們不確定這將在何時(shí)成為主要治療方法,但該技術(shù)的未來(lái)是非常激動(dòng)人心的。”
3D打印的優(yōu)勢(shì)
維克森林大學(xué)的科學(xué)家多年來(lái)一直在實(shí)驗(yàn)室培育器官和組織。他們?cè)趯?shí)驗(yàn)室里用3D打印技術(shù)制造了一個(gè)迷你腎臟和一個(gè)迷你肝臟。下一個(gè)挑戰(zhàn):更大的、可以更充分地模擬器官功能的實(shí)心結(jié)構(gòu)。“在器官尺寸上,我們離實(shí)現(xiàn)這一目標(biāo)還有很長(zhǎng)一段路要走。”哈佛大學(xué)(Harvard University)懷斯生物啟發(fā)工程研究所(Biologically Inspired Engineering)的教授詹妮弗·劉易斯表示。
“我們已經(jīng)能夠打印出像皮膚這樣的平面結(jié)構(gòu),像血管這樣的管狀結(jié)構(gòu),或者像膀胱這樣的空心非管狀器官。”維克森林研究所的創(chuàng)始主任安東尼·阿塔拉說(shuō)。“由于血管和營(yíng)養(yǎng)方面的挑戰(zhàn)”,打印更大的實(shí)心器官是不同的,畢竟“每厘米就有非常多細(xì)胞。”
在細(xì)胞制造的某些方面,還存在質(zhì)量問(wèn)題。科學(xué)家們已經(jīng)可以從干細(xì)胞中制造出心肌細(xì)胞,但制造出的心肌細(xì)胞無(wú)法像你的心肌細(xì)胞那樣強(qiáng)烈地跳動(dòng)。肝細(xì)胞(代謝)和腎細(xì)胞(濾液攝取)的情況也是如此。斯凱拉-斯科特稱:“從某些方面講,3D生物打印領(lǐng)域正在等待基礎(chǔ)生物學(xué)家取得重大突破。”
還有一個(gè)問(wèn)題是數(shù)量問(wèn)題。制造一顆心臟需要“數(shù)十億個(gè)細(xì)胞——而且需要不同的細(xì)胞,甚至是不同的心肌細(xì)胞。”塔爾·德維爾說(shuō)道。根據(jù)斯凱拉-斯科特的說(shuō)法,要為一個(gè)器官制造足夠的細(xì)胞,制造廠需要一個(gè)10升的攪拌缸,每天可能要花費(fèi)5,000美元,而且需要連續(xù)幾個(gè)月才能夠完成。最終目標(biāo)是每個(gè)月培育上千個(gè)器官,而不是一個(gè)器官。
3D Bio Therapeutics的首席執(zhí)行官及聯(lián)合創(chuàng)始人丹·科恩表示,除此之外,還有組織如何融入人體以及如何得到人體的支持等問(wèn)題,包括復(fù)雜的血管、神經(jīng)和多種細(xì)胞類型網(wǎng)絡(luò)。“這并不是說(shuō)這一點(diǎn)無(wú)法做到。”科恩說(shuō),他20年前就開(kāi)始在生物打印領(lǐng)域工作,當(dāng)時(shí)這個(gè)領(lǐng)域連個(gè)正式的名字都沒(méi)有。“我對(duì)生物打印和再生醫(yī)學(xué)的廣泛應(yīng)用抱有很大希望。”
就短期而言,進(jìn)展也是非常顯著的。劉易斯表示,哈佛大學(xué)的研究人員從人類多能干細(xì)胞中培育出心肌細(xì)胞,然后將它們植入帶有傳感器(這些傳感器可以追蹤跳動(dòng)的組織)的生物工程芯片上。這種3D打印的芯片上的心臟能夠用于測(cè)試各種心臟藥物的潛在毒副作用,并可能減輕對(duì)動(dòng)物試驗(yàn)的需求。(類似的芯片上的肌萎縮性側(cè)索硬化癥技術(shù)正在被用于篩選候選藥物,這樣也可以更好地了解這種疾病的潛在機(jī)制。)
維克森林大學(xué)的阿塔拉說(shuō):“3D打印機(jī)有幾大優(yōu)點(diǎn)。首先是能夠擴(kuò)大規(guī)模,因?yàn)槟憧梢杂么蛴C(jī)自動(dòng)化打印(組織和器官),而不是手工一次完成一個(gè)。其次是能夠確保精確度。我們可以更精確地將細(xì)胞放置在需要它們的地方。”
再有一點(diǎn)就是能夠降低整體成本,這是因?yàn)?D打印允許加大規(guī)模。這就是阿塔拉所說(shuō)的“可重復(fù)性”(一種可以反復(fù)制造相同結(jié)構(gòu)的方法)。在器官移植方面,由患者自身細(xì)胞制成的新器官能夠大大降低排異反應(yīng)的可能性。
大多數(shù)研究人員認(rèn)為,全尺寸3D打印人體器官移植還需要20年到30年的時(shí)間。“展望未來(lái),我們將無(wú)需接受心臟捐贈(zèng),也無(wú)需接受肝臟捐贈(zèng)。”德維爾說(shuō)。“這是我的觀點(diǎn),而且我很樂(lè)觀,我認(rèn)為在不到20年的時(shí)間里,就會(huì)出現(xiàn)打印的器官被植入患者體內(nèi)。”這是科學(xué)在發(fā)揮作用,而不是科幻小說(shuō)。(財(cái)富中文網(wǎng))
譯者:中慧言-王芳
Last year, in San Antonio, Texas, Dr. Arturo Bonilla carefully implanted an outer ear on a 20-year-old woman born without one. The ear on the woman’s right side, had been constructed in the size and shape of her left.
For Bonilla, a pediatric microtia surgeon (a doctor who treats birth defects of the ear) for more than 25 years and a recognized expert in the field, such a procedure would normally be routine. But this case had a twist: For the first time, the ear he was implanting was the product of a 3D bioprinter using the woman’s own cartilage cells.
The implant procedure, Bonilla told me, was “very uneventful.” It is a vast understatement, all things considered.
From the realm of near-fiction to the germ of an idea to actual science, 3D bioprinting is advancing across all aspects of medical research—and, now, practice. The pace is slow, and target dates for some of the most ambitious 3D plans are decades off. But progress is real.
“I think that in 10 years we will have organs for transplantation,” says professor Tal Dvir, director of tissue engineering and regenerative medicine at Tel Aviv University in Israel. “We will start with simple organs like skin and cartilage, but then we’ll move on to more complicated tissues—eventually the heart, liver, kidney.”
The future of 3D bioprinting
It sounds fantastical, but it’s already happening. Multilayered skin, bones, muscle structures, blood vessels, retinal tissue and even mini-organs all have been 3D printed. While none of the printed products are yet approved for human use, the race up the scientific timeline is breathtaking—and Bonilla’s ear procedure, the first 3D bioprint from live cells to be implanted in a human, marks a significant moment along that progression.
Researchers in Poland bioprinted a functional prototype of a pancreas in which stable blood flow was achieved in pigs during an observed two-week period, according to a 2022 abstract and Dr. Michal Wszola, creator of Bionic Pancreas. United Therapeutics Corporation has 3D printed a human lung scaffold with 4,000 kilometers of capillaries and 200 million alveoli (tiny air sacs) that are capable of oxygen exchange in animal models—a critical step toward creating tolerable, transplantable human lungs with the goal of being cleared for human trials within five years.
At Wake Forest University Institute for Regenerative Medicine, scientists have developed a mobile skin bioprinting system. In the not-too-distant future, they anticipate being able to roll the printer right to the bedside of a patient suffering from a non-healing wound, such as a burn, then scan and measure the wound area and 3D print skin, layer by layer, directly onto the wound surface. And they’ve gone deeper, 3D printing skeletal muscle constructs that have been shown to contract in rodents and regain more than 80% of previously lost muscular function in an anterior leg muscle within eight weeks.
Dvir’s own lab has produced a 3D-printed “rabbit-sized” heart, as he puts it, replete with cells, chambers, the major blood vessels and a heartbeat. Full scale human hearts, the professor notes, require the same basic technology, although the process of scaling up is vastly complicated. “We’re now working on the pacemaker cells, the atrial cells, the ventricular cells,” Dvir says. “But it looks good. I believe this is the future.”
How 3D bioprinting works
The ability to 3D print human organs is an astounding notion. Nearly 106,000 Americans are currently on waiting lists for organ donations, and 17 die each day while waiting, according to the federal Health Resources and Services Administration. A 3D printing process that uses the patient’s own cells to grow organs would not only potentially curb that waiting list, but dramatically reduce the chances of organ rejection and likely eliminate the need for harmful life-long immunosuppressive medication.
“The ability to place different cell types in precise locations to build up a complex tissue, and the capability of integrating blood vessels that can deliver the necessary oxygen and nutrients to keep cells alive, are two (3D) techniques that are revolutionizing tissue engineering,” says Mark Skylar-Scott, an assistant professor in the Stanford University department of bioengineering. “The field has moved very quickly over the past two decades, from printed bladders to now highly cellular tissues with vessels that can be connected to a pump—and complex 3D models that resemble heart components with integrated heart cells.”
In 3D bioprinting, the name of the game is cells. The process begins by generating the cells that researchers want to bioprint, which are then instructed to become organ specific cell types. The cells are then rendered into a printable living ink, or bioink, that involves mixing them with materials like gelatin or alginate to give them a toothpaste-like consistency. Stanford’s lab is studying how stem cells might naturally form such a consistency if crammed together at high density, which could lead to 3D printed organs made strictly from a patient’s own cells.
The bioink is loaded into syringes and squeezed out of a nozzle “l(fā)ike icing on a cake,” Skylar-Scott says. This is the actual 3D bioprinting process, and it typically involves laying down different cell types, each loaded into a different nozzle. (Dvir says the mini-heart took about four hours to print.) Once it is finished, the tissue is sometimes connected to a pump that drives oxygen and nutrients through it. Given time, the tissue develops on its own and increases in both maturity and function.
That general process, though dramatically oversimplified here, is what led to the production of the external part of the ear that Arturo Bonilla implanted in his patient in Texas. In most previous microtia surgeries, Bonilla would have carved a new ear out of cartilage taken from the patient’s ribs. Instead, a small biopsy was performed on the patient’s other ear and cartilage cells taken from the biopsy were grown into billions of cells, which were 3D-printed into the new implant.
“As with any study, there will likely be iterations in future patients in order to try to improve this technique,” Bonilla says. “We are unsure when this will be the mainstay treatment, but the future is very exciting.”
Advantages of 3D printing
Wake Forest scientists have been lab growing organs and tissues for years. They’ve used 3D printing to create in the laboratory essentially a mini-kidney and a mini-liver. The next challenge: larger, solid structures that more fully mimic organ function. “We are far from achieving this goal at organ scale,” says Jennifer Lewis, Wyss Professor of Biologically Inspired Engineering, at Harvard University.
“We’ve been able to print flat structures like skin, tubular structures like blood vessels or hollow, non-tubular organs like a bladder,” says Anthony Atala, founding director of the Wake Forest Institute. The larger solid organs are different, Atala says, “because of the challenge with the vascularity or the nutrition. There’s so many cells per centimeter.”
In some ways with cell production, it’s a matter of quality. Scientists have been able to create a heart cell from stem cells, but not one that beats as strongly as your heart cells do. The same is true for liver cells (metabolism) and kidney cells (filtrate uptake). “In some ways,” Skyler-Scott says, “the 3D bioprinting field is waiting on the basic biologists to make their major breakthroughs.”
There’s also the issue of quantity. The creation of a heart would require “billions of cells – and you need different cells, even different cardiac cells,” says Tal Dvir. To make enough cells for a single organ, a facility would need a 10-liter stirred vat that might cost $5,000 per day to feed, for months on end according to Skyler-Scott. And the ultimate goal is thousands of organs a month, not one.
Beyond all that, there are the questions of how the tissue integrates into the body and how it is supported by the body, including complex networks of blood vessels, nerves and multiple cell types, says Dan Cohen, CEO and co-founder of 3D Bio Therapeutics. “It’s not to say it can’t be done,” says Cohen, who began working in the field of bioprinting 20 years ago, when it didn’t have a formal name. “I have a lot of hope for bioprinting and regenerative medicine more broadly.”
Even in the short term, progress is well marked. Researchers at Harvard, Lewis says, generated cardiac cells from human pluripotent stem cells, then seeded them on a bioengineered chip with integrated sensors that can track the beating tissue. This 3D-printed-heart-on-a-chip can be used to test various cardiac drugs for potentially toxic side effects and may alleviate the need for animal testing.(A similar ALS-on-a-chip?technology is being used to screen for drug candidates and to better understand the underlying mechanisms of that disease.)
“The 3D printer gives you several advantages,” says Wake Forest’s Atala. “The first is scale-up, because instead of making these (tissues and organs) by hand one at a time, you can automate the printer to do it. The second thing is precision. We can more precisely locate the cells where they’re needed.”
There’s also the notion of lower overall cost, as 3D printing allows for that increased scale. There is what Atala calls “reproducibility,” a method of producing the same structure again and again. And in terms of organ transplant, a new organ made of a patient’s own cells makes rejection far less likely.
Most researchers put the idea of full-sized 3D-printed organ transplantation in humans at somewhere between 20 and 30 years away. “Eventually, looking ahead, we’ll not need donor hearts. We’ll not need livers,” Dvir says. “This is my opinion, and I’m optimistic, but I think that in less than 20 years we will have printed organs inside us.” That is science at work, not science fiction.






